Define Periodontal Disease by Its Pathogens
Periodontal disease by definition is an infectious, contagious, inflammatory, polymicrobial disease with systemic and genetic expression.
More resources on periodontal disease and oral pathogens can be found in AAOSH Core Curriculum. Free for AAOSH Members. Learn more about AAOSH membership here!
Stay up to date on AAOSH articles,
resources, events, and more by subscribing here
defining periodontal disease by it's pathogens
Polymicrobial means many strains of pathogens are present. Each strain presents with different sensitivities to different antimicrobials or antibiotics. It becomes relevant to treating pathogenic infections to know what strains are present to become aware of how best to plan a treatment remedy. The stains present can be determined by a simple saliva test. This test is used to determine the pathogens present and the concentration of those pathogens. The prescribing dentist determines the appropriate periodontal therapy depending on the results of the saliva test. The patient’s dental and medical history will be considered when evaluating the use of antibiotic medications to treat the periodontal condition. There are different antibiotic options depending on which pathogens are present and the concentration of those pathogens.
Know the Types of Oral Pathogens
 Of the more than 800 oral bacteria, at least 11 pathogens are also found systemically and can be identified routinely by both their individual strain and their concentration via a simple bacterial DNA test.
Of the more than 800 oral bacteria, at least 11 pathogens are also found systemically and can be identified routinely by both their individual strain and their concentration via a simple bacterial DNA test.
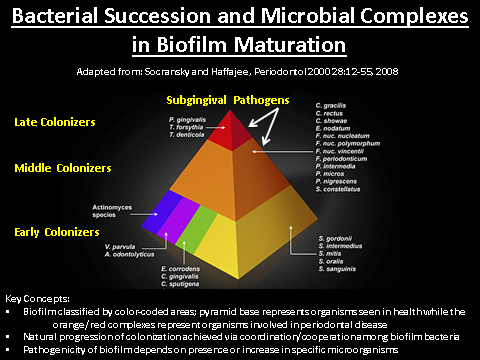
Four of the most virulent and destructive periodontal pathogens are Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia. In salivary pathogen testing and much literature, they are referred to as the red complex, high-risk, or late colonizing pathogens. The high-risk pathogens are initiators of intracellular damage wherever they are found.
There are six moderate-risk pathogens: Eubacterium nucleaturm, Fusobcterium nucleatum, Prevotella intermedia, Campylobacter rectus, Peptostreptococcus micros, and Eikenella corrodens. This group is known as the orange complex or middle colonizing pathogens, and they are usually collaborative once a red complex organism has entered a cell. Many recent studies are finding that F. nucleatum and C. rectus can be found alone and are seemingly solely responsible for an inflammatory response.
The last pathogen is Campylobacter showae, a low-risk, early colonizing or “green complex” bacteria. It also is collaborative and has been found to be of far less threat systemically than the others.
The Effect on Oral Health
All of the systemically virulent pathogens from periodontal disease are pathogenic, relative to their individual or collective concentrations or to their total numbers. Certainly, there are times for all individuals when each of the strains is present 100% of the time. It is only when genetics, low immunity, low resistance, or chronically uninterrupted colonies are allowed to proliferate that total counts elevate to encourage systemic infection.
The systemic impact of periodontal pathogens is profound. Periodontal pathogens are associated with or linked to 16 systemic diseases to date, including cardiovascular disease, diabetes, respiratory disease, chronic obstructive pulmonary disease, rheumatoid arthritis, gastrointestinal disorders, Alzheimer’s disease, osteoporosis, kidney disease, preterm birth, preterm birth weight, and cancer. Periodontal disease treatment, then, must be considered a part of the preventive armamentarium for chronic disease management.
Perhaps looking at dentists as doctors of oral medicine, hygienists as oral medicine therapists, dental assistants as oral medicine technicians, and the administrative team members as oral medicine facilitators will bring into focus exactly what dental professionals are responsible for. Dentistry is moving beyond saving a tooth and moving closer to saving and extending lives.
Interested in learning more? Join The American Academy for Oral Systemic Health for Collaboration Cures 2022 in Phoenix, AZ. Sign up for updates and more information here.
Collaboration Cures 2022 is a collaborative meeting bringing together speakers, research, and practitioners from all health fields to hear the latest in oral systemic health, myofunctional therapy, nutrition, physical therapy, and more.
Ms. Warner is a practicing hygienist, an oral medicine coach and facilitator and a former adjunct professor at Baker College of Cadillac, Mich. She graduated from the Ferris State University School of Dental Hygiene and completed studies with Dawson Academy’s Dental Institute for Systemic Health. Also, she is a member of the American Academy for Oral Systemic Health. Throughout her 30-year career as a dental hygienist, she observed the connection between oral and systemic health in her patients, proactively partnering with them to better manage their total wellness. Her mission is to raise awareness of oral health as a crucial part of an integrated approach to whole-body wellness. She can be reached at traci@extraordinarypractice.com.


